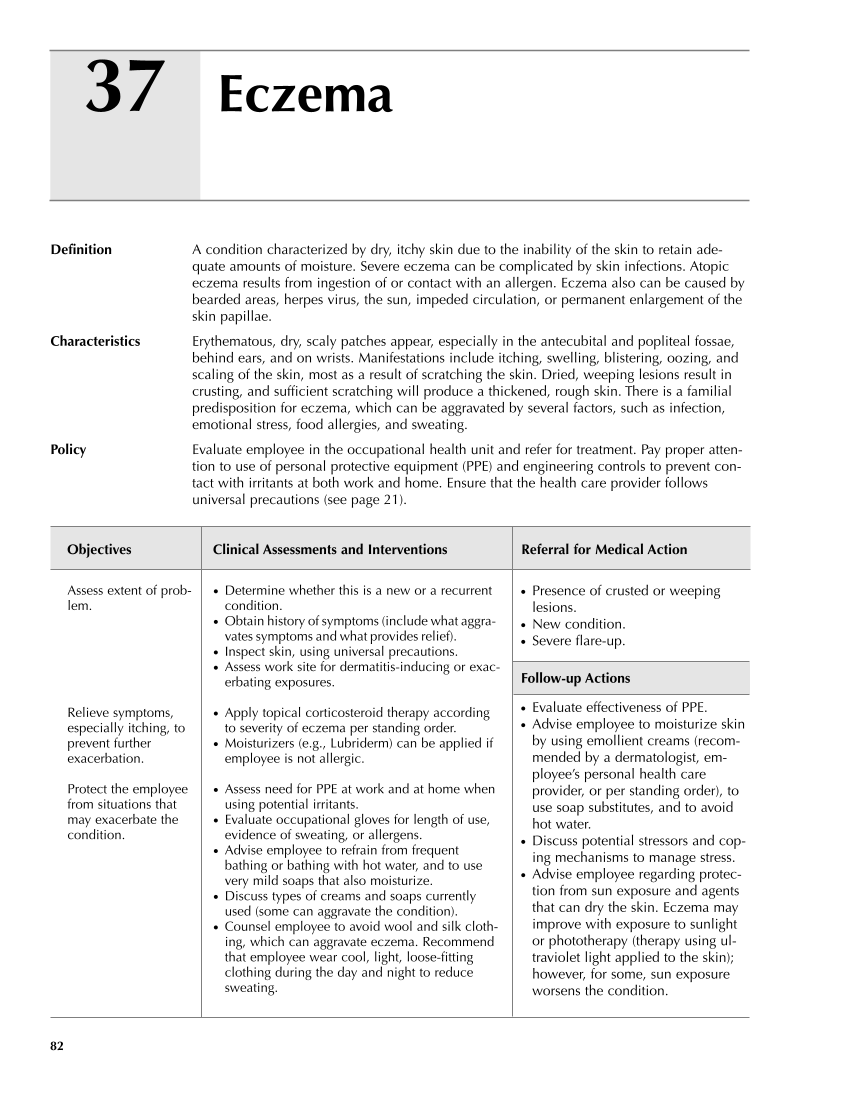
37 82 Definition A condition characterized by dry, itchy skin due to the inability of the skin to retain ade- quate amounts of moisture. Severe eczema can be complicated by skin infections. Atopic eczema results from ingestion of or contact with an allergen. Eczema also can be caused by bearded areas, herpes virus, the sun, impeded circulation, or permanent enlargement of the skin papillae. Characteristics Erythematous, dry, scaly patches appear, especially in the antecubital and popliteal fossae, behind ears, and on wrists. Manifestations include itching, swelling, blistering, oozing, and scaling of the skin, most as a result of scratching the skin. Dried, weeping lesions result in crusting, and sufficient scratching will produce a thickened, rough skin. There is a familial predisposition for eczema, which can be aggravated by several factors, such as infection, emotional stress, food allergies, and sweating. Policy Evaluate employee in the occupational health unit and refer for treatment. Pay proper atten- tion to use of personal protective equipment (PPE) and engineering controls to prevent con- tact with irritants at both work and home. Ensure that the health care provider follows universal precautions (see page 21). Objectives Clinical Assessments and Interventions Referral for Medical Action Eczema ● Presence of crusted or weeping lesions. ● New condition. ● Severe flare-up. Follow-up Actions ● Evaluate effectiveness of PPE. ● Advise employee to moisturize skin by using emollient creams (recom- mended by a dermatologist, em- ployee’s personal health care provider, or per standing order), to use soap substitutes, and to avoid hot water. ● Discuss potential stressors and cop- ing mechanisms to manage stress. ● Advise employee regarding protec- tion from sun exposure and agents that can dry the skin. Eczema may improve with exposure to sunlight or phototherapy (therapy using ul- traviolet light applied to the skin) however, for some, sun exposure worsens the condition. Assess extent of prob- lem. Relieve symptoms, especially itching, to prevent further exacerbation. Protect the employee from situations that may exacerbate the condition. ● Determine whether this is a new or a recurrent condition. ● Obtain history of symptoms (include what aggra- vates symptoms and what provides relief). ● Inspect skin, using universal precautions. ● Assess work site for dermatitis-inducing or exac- erbating exposures. ● Apply topical corticosteroid therapy according to severity of eczema per standing order. ● Moisturizers (e.g., Lubriderm) can be applied if employee is not allergic. ● Assess need for PPE at work and at home when using potential irritants. ● Evaluate occupational gloves for length of use, evidence of sweating, or allergens. ● Advise employee to refrain from frequent bathing or bathing with hot water, and to use very mild soaps that also moisturize. ● Discuss types of creams and soaps currently used (some can aggravate the condition). ● Counsel employee to avoid wool and silk cloth- ing, which can aggravate eczema. Recommend that employee wear cool, light, loose-fitting clothing during the day and night to reduce sweating. Guideline continues on next page
Purchased from OEM Press by (ge corporate access). (C) 2013 OEM Health Information, Inc. All rights reserved.