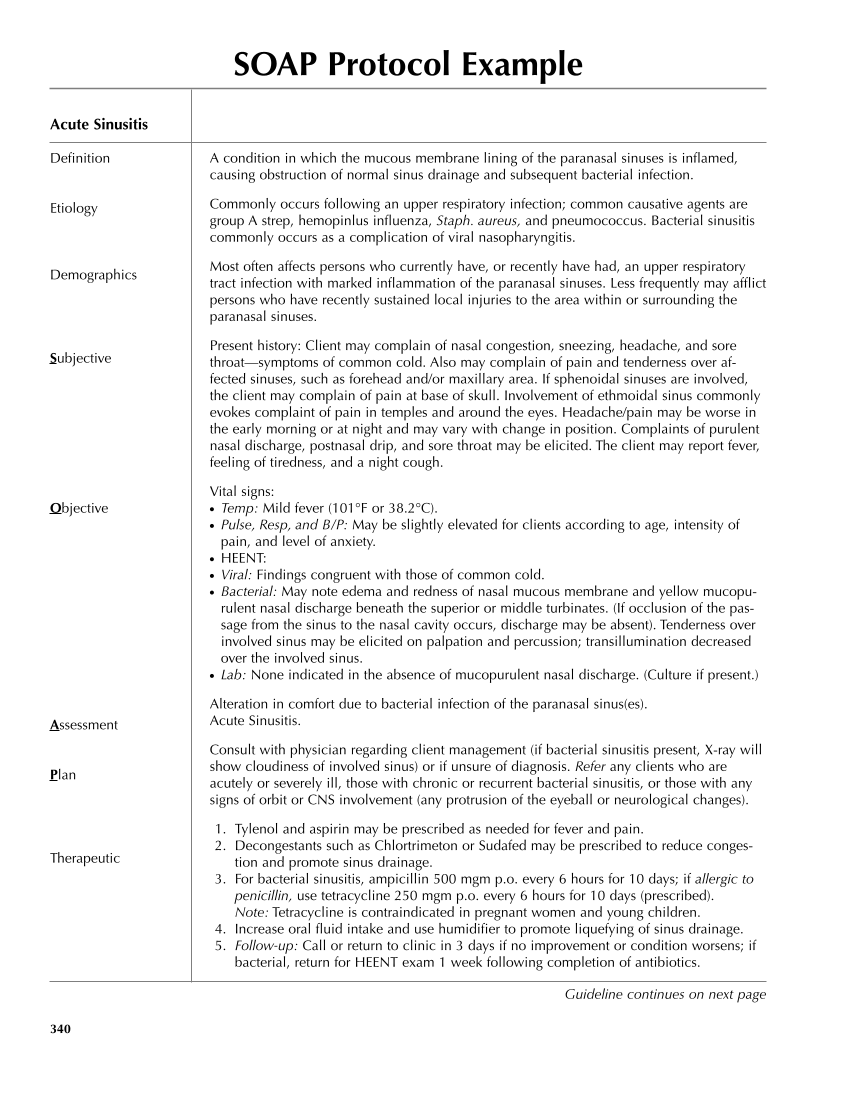
SOAP Protocol Example Acute Sinusitis Definition Etiology Demographics Subjective Objective Assessment Plan Therapeutic 340 A condition in which the mucous membrane lining of the paranasal sinuses is inflamed, causing obstruction of normal sinus drainage and subsequent bacterial infection. Commonly occurs following an upper respiratory infection common causative agents are group A strep, hemopinlus influenza, Staph. aureus, and pneumococcus. Bacterial sinusitis commonly occurs as a complication of viral nasopharyngitis. Most often affects persons who currently have, or recently have had, an upper respiratory tract infection with marked inflammation of the paranasal sinuses. Less frequently may afflict persons who have recently sustained local injuries to the area within or surrounding the paranasal sinuses. Present history: Client may complain of nasal congestion, sneezing, headache, and sore throat—symptoms of common cold. Also may complain of pain and tenderness over af- fected sinuses, such as forehead and/or maxillary area. If sphenoidal sinuses are involved, the client may complain of pain at base of skull. Involvement of ethmoidal sinus commonly evokes complaint of pain in temples and around the eyes. Headache/pain may be worse in the early morning or at night and may vary with change in position. Complaints of purulent nasal discharge, postnasal drip, and sore throat may be elicited. The client may report fever, feeling of tiredness, and a night cough. Vital signs: ● Temp: Mild fever (101°F or 38.2°C). ● Pulse, Resp, and B/P: May be slightly elevated for clients according to age, intensity of pain, and level of anxiety. ● HEENT: ● Viral: Findings congruent with those of common cold. ● Bacterial: May note edema and redness of nasal mucous membrane and yellow mucopu- rulent nasal discharge beneath the superior or middle turbinates. (If occlusion of the pas- sage from the sinus to the nasal cavity occurs, discharge may be absent). Tenderness over involved sinus may be elicited on palpation and percussion transillumination decreased over the involved sinus. ● Lab: None indicated in the absence of mucopurulent nasal discharge. (Culture if present.) Alteration in comfort due to bacterial infection of the paranasal sinus(es). Acute Sinusitis. Consult with physician regarding client management (if bacterial sinusitis present, X-ray will show cloudiness of involved sinus) or if unsure of diagnosis. Refer any clients who are acutely or severely ill, those with chronic or recurrent bacterial sinusitis, or those with any signs of orbit or CNS involvement (any protrusion of the eyeball or neurological changes). 1. Tylenol and aspirin may be prescribed as needed for fever and pain. 2. Decongestants such as Chlortrimeton or Sudafed may be prescribed to reduce conges- tion and promote sinus drainage. 3. For bacterial sinusitis, ampicillin 500 mgm p.o. every 6 hours for 10 days if allergic to penicillin, use tetracycline 250 mgm p.o. every 6 hours for 10 days (prescribed). Note: Tetracycline is contraindicated in pregnant women and young children. 4. Increase oral fluid intake and use humidifier to promote liquefying of sinus drainage. 5. Follow-up: Call or return to clinic in 3 days if no improvement or condition worsens if bacterial, return for HEENT exam 1 week following completion of antibiotics. Guideline continues on next page
Purchased from OEM Press by (ge corporate access). (C) 2013 OEM Health Information, Inc. All rights reserved.