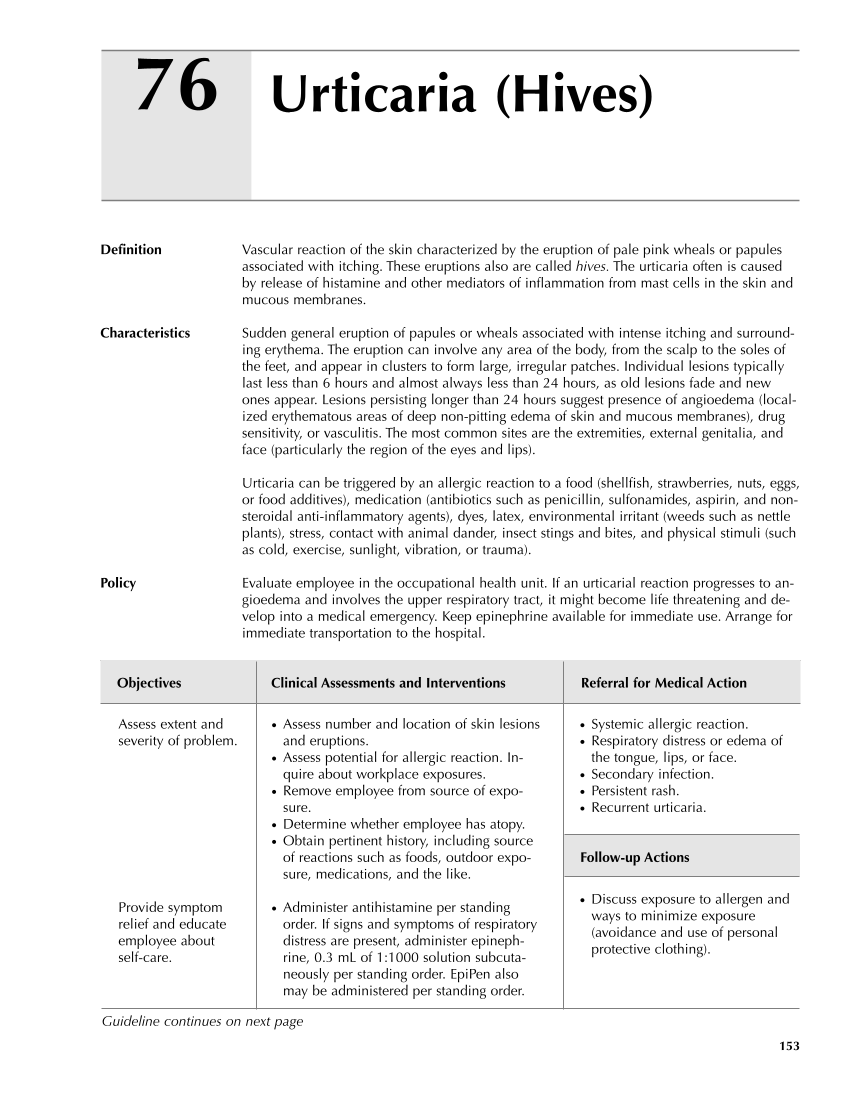
● Systemic allergic reaction. ● Respiratory distress or edema of the tongue, lips, or face. ● Secondary infection. ● Persistent rash. ● Recurrent urticaria. Follow-up Actions ● Discuss exposure to allergen and ways to minimize exposure (avoidance and use of personal protective clothing). Assess extent and severity of problem. Provide symptom relief and educate employee about self-care. ● Assess number and location of skin lesions and eruptions. ● Assess potential for allergic reaction. In- quire about workplace exposures. ● Remove employee from source of expo- sure. ● Determine whether employee has atopy. ● Obtain pertinent history, including source of reactions such as foods, outdoor expo- sure, medications, and the like. ● Administer antihistamine per standing order. If signs and symptoms of respiratory distress are present, administer epineph- rine, 0.3 mL of 1:1000 solution subcuta- neously per standing order. EpiPen also may be administered per standing order. 153 Urticaria (Hives) 76 Definition Vascular reaction of the skin characterized by the eruption of pale pink wheals or papules associated with itching. These eruptions also are called hives. The urticaria often is caused by release of histamine and other mediators of inflammation from mast cells in the skin and mucous membranes. Characteristics Sudden general eruption of papules or wheals associated with intense itching and surround- ing erythema. The eruption can involve any area of the body, from the scalp to the soles of the feet, and appear in clusters to form large, irregular patches. Individual lesions typically last less than 6 hours and almost always less than 24 hours, as old lesions fade and new ones appear. Lesions persisting longer than 24 hours suggest presence of angioedema (local- ized erythematous areas of deep non-pitting edema of skin and mucous membranes), drug sensitivity, or vasculitis. The most common sites are the extremities, external genitalia, and face (particularly the region of the eyes and lips). Urticaria can be triggered by an allergic reaction to a food (shellfish, strawberries, nuts, eggs, or food additives), medication (antibiotics such as penicillin, sulfonamides, aspirin, and non- steroidal anti-inflammatory agents), dyes, latex, environmental irritant (weeds such as nettle plants), stress, contact with animal dander, insect stings and bites, and physical stimuli (such as cold, exercise, sunlight, vibration, or trauma). Policy Evaluate employee in the occupational health unit. If an urticarial reaction progresses to an- gioedema and involves the upper respiratory tract, it might become life threatening and de- velop into a medical emergency. Keep epinephrine available for immediate use. Arrange for immediate transportation to the hospital. Objectives Clinical Assessments and Interventions Referral for Medical Action Guideline continues on next page
Purchased from OEM Press by (ge corporate access). (C) 2013 OEM Health Information, Inc. All rights reserved.