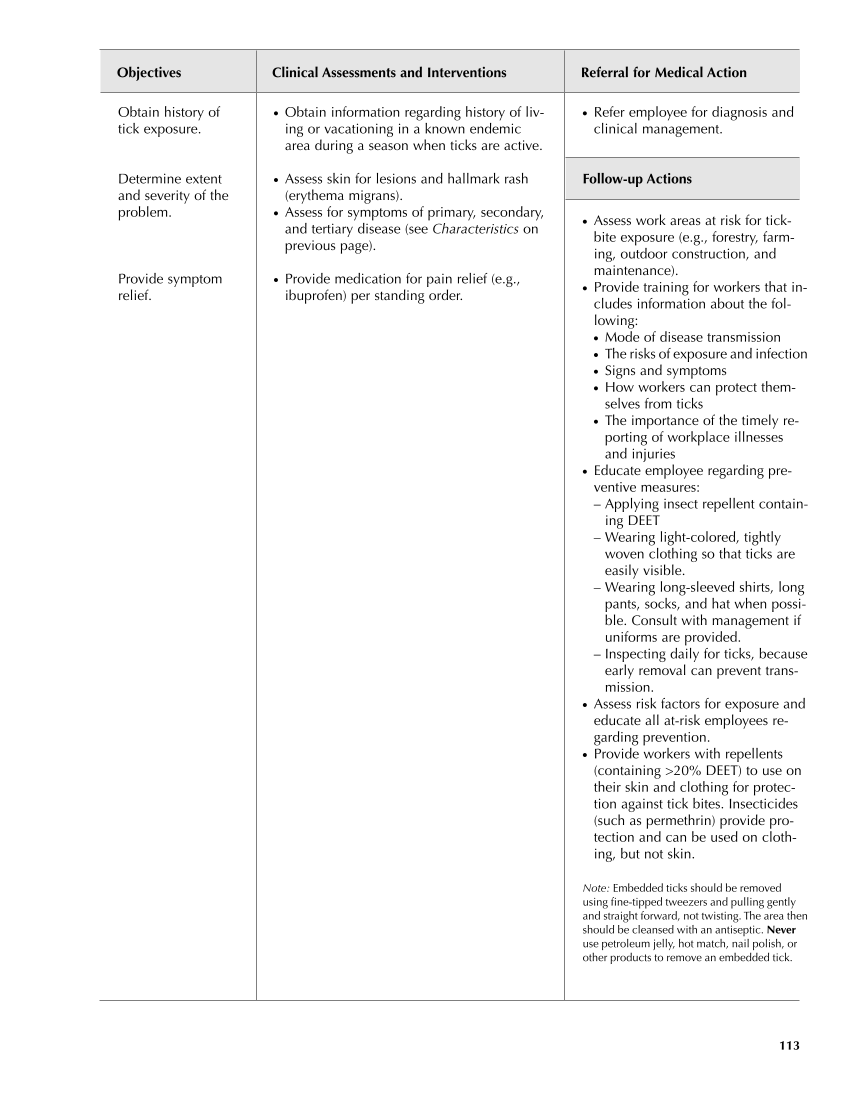
● Refer employee for diagnosis and clinical management. Follow-up Actions ● Assess work areas at risk for tick- bite exposure (e.g., forestry, farm- ing, outdoor construction, and maintenance). ● Provide training for workers that in- cludes information about the fol- lowing: ● Mode of disease transmission ● The risks of exposure and infection ● Signs and symptoms ● How workers can protect them- selves from ticks ● The importance of the timely re- porting of workplace illnesses and injuries ● Educate employee regarding pre- ventive measures: – Applying insect repellent contain- ing DEET – Wearing light-colored, tightly woven clothing so that ticks are easily visible. – Wearing long-sleeved shirts, long pants, socks, and hat when possi- ble. Consult with management if uniforms are provided. – Inspecting daily for ticks, because early removal can prevent trans- mission. ● Assess risk factors for exposure and educate all at-risk employees re- garding prevention. ● Provide workers with repellents (containing 20% DEET) to use on their skin and clothing for protec- tion against tick bites. Insecticides (such as permethrin) provide pro- tection and can be used on cloth- ing, but not skin. Note: Embedded ticks should be removed using fine-tipped tweezers and pulling gently and straight forward, not twisting. The area then should be cleansed with an antiseptic. Never use petroleum jelly, hot match, nail polish, or other products to remove an embedded tick. Objectives Clinical Assessments and Interventions Referral for Medical Action 113 Obtain history of tick exposure. Determine extent and severity of the problem. Provide symptom relief. ● Obtain information regarding history of liv- ing or vacationing in a known endemic area during a season when ticks are active. ● Assess skin for lesions and hallmark rash (erythema migrans). ● Assess for symptoms of primary, secondary, and tertiary disease (see Characteristics on previous page). ● Provide medication for pain relief (e.g., ibuprofen) per standing order.
Purchased from OEM Press by (ge corporate access). (C) 2013 OEM Health Information, Inc. All rights reserved.