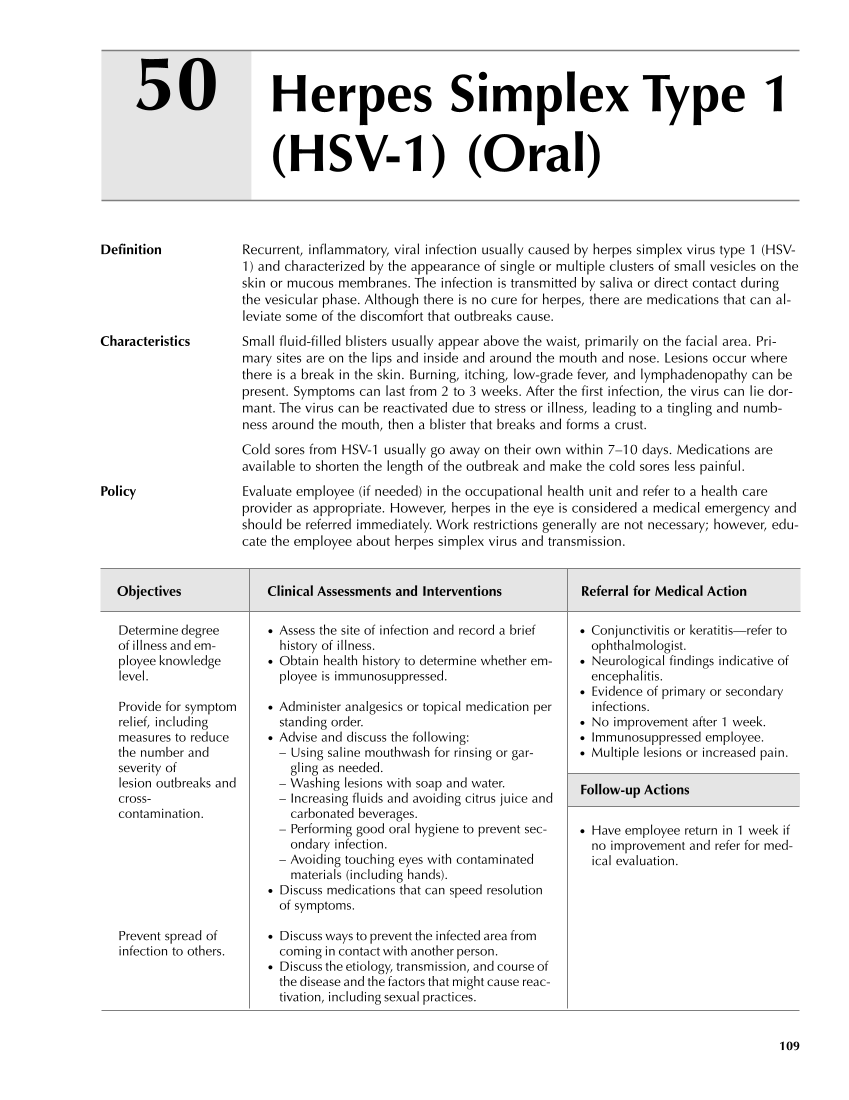
109 Herpes Simplex Type 1 (HSV-1) (Oral) 50 Definition Recurrent, inflammatory, viral infection usually caused by herpes simplex virus type 1 (HSV- 1) and characterized by the appearance of single or multiple clusters of small vesicles on the skin or mucous membranes. The infection is transmitted by saliva or direct contact during the vesicular phase. Although there is no cure for herpes, there are medications that can al- leviate some of the discomfort that outbreaks cause. Characteristics Small fluid-filled blisters usually appear above the waist, primarily on the facial area. Pri- mary sites are on the lips and inside and around the mouth and nose. Lesions occur where there is a break in the skin. Burning, itching, low-grade fever, and lymphadenopathy can be present. Symptoms can last from 2 to 3 weeks. After the first infection, the virus can lie dor- mant. The virus can be reactivated due to stress or illness, leading to a tingling and numb- ness around the mouth, then a blister that breaks and forms a crust. Cold sores from HSV-1 usually go away on their own within 7–10 days. Medications are available to shorten the length of the outbreak and make the cold sores less painful. Policy Evaluate employee (if needed) in the occupational health unit and refer to a health care provider as appropriate. However, herpes in the eye is considered a medical emergency and should be referred immediately. Work restrictions generally are not necessary however, edu- cate the employee about herpes simplex virus and transmission. Objectives Clinical Assessments and Interventions Referral for Medical Action ● Conjunctivitis or keratitis—refer to ophthalmologist. ● Neurological findings indicative of encephalitis. ● Evidence of primary or secondary infections. ● No improvement after 1 week. ● Immunosuppressed employee. ● Multiple lesions or increased pain. Follow-up Actions ● Have employee return in 1 week if no improvement and refer for med- ical evaluation. Determine degree of illness and em- ployee knowledge level. Provide for symptom relief, including measures to reduce the number and severity of lesion outbreaks and cross- contamination. Prevent spread of infection to others. ● Assess the site of infection and record a brief history of illness. ● Obtain health history to determine whether em- ployee is immunosuppressed. ● Administer analgesics or topical medication per standing order. ● Advise and discuss the following: – Using saline mouthwash for rinsing or gar- gling as needed. – Washing lesions with soap and water. – Increasing fluids and avoiding citrus juice and carbonated beverages. – Performing good oral hygiene to prevent sec- ondary infection. – Avoiding touching eyes with contaminated materials (including hands). ● Discuss medications that can speed resolution of symptoms. ● Discuss ways to prevent the infected area from coming in contact with another person. ● Discuss the etiology, transmission, and course of the disease and the factors that might cause reac- tivation, including sexual practices. Guideline continues on next page
Purchased from OEM Press by (ge corporate access). (C) 2013 OEM Health Information, Inc. All rights reserved.