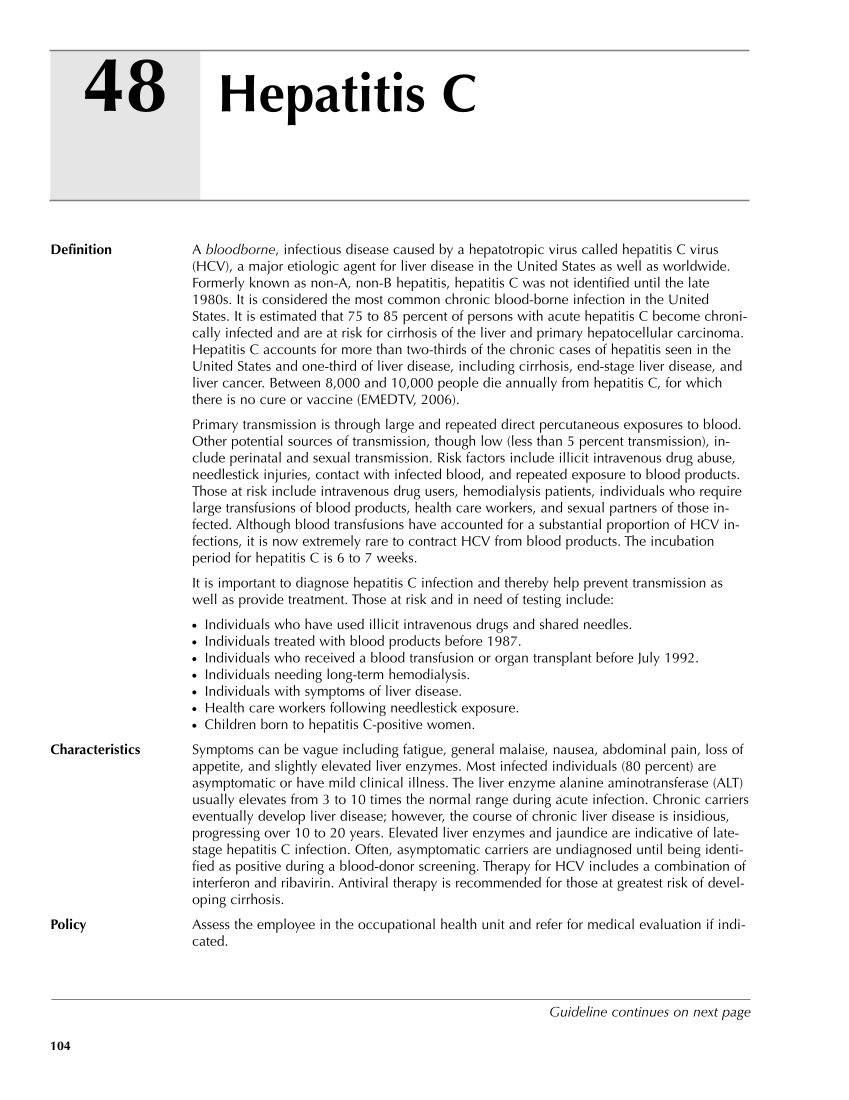
48 104 Definition A bloodborne, infectious disease caused by a hepatotropic virus called hepatitis C virus (HCV), a major etiologic agent for liver disease in the United States as well as worldwide. Formerly known as non-A, non-B hepatitis, hepatitis C was not identified until the late 1980s. It is considered the most common chronic blood-borne infection in the United States. It is estimated that 75 to 85 percent of persons with acute hepatitis C become chroni- cally infected and are at risk for cirrhosis of the liver and primary hepatocellular carcinoma. Hepatitis C accounts for more than two-thirds of the chronic cases of hepatitis seen in the United States and one-third of liver disease, including cirrhosis, end-stage liver disease, and liver cancer. Between 8,000 and 10,000 people die annually from hepatitis C, for which there is no cure or vaccine (EMEDTV, 2006). Primary transmission is through large and repeated direct percutaneous exposures to blood. Other potential sources of transmission, though low (less than 5 percent transmission), in- clude perinatal and sexual transmission. Risk factors include illicit intravenous drug abuse, needlestick injuries, contact with infected blood, and repeated exposure to blood products. Those at risk include intravenous drug users, hemodialysis patients, individuals who require large transfusions of blood products, health care workers, and sexual partners of those in- fected. Although blood transfusions have accounted for a substantial proportion of HCV in- fections, it is now extremely rare to contract HCV from blood products. The incubation period for hepatitis C is 6 to 7 weeks. It is important to diagnose hepatitis C infection and thereby help prevent transmission as well as provide treatment. Those at risk and in need of testing include: ● Individuals who have used illicit intravenous drugs and shared needles. ● Individuals treated with blood products before 1987. ● Individuals who received a blood transfusion or organ transplant before July 1992. ● Individuals needing long-term hemodialysis. ● Individuals with symptoms of liver disease. ● Health care workers following needlestick exposure. ● Children born to hepatitis C-positive women. Characteristics Symptoms can be vague including fatigue, general malaise, nausea, abdominal pain, loss of appetite, and slightly elevated liver enzymes. Most infected individuals (80 percent) are asymptomatic or have mild clinical illness. The liver enzyme alanine aminotransferase (ALT) usually elevates from 3 to 10 times the normal range during acute infection. Chronic carriers eventually develop liver disease however, the course of chronic liver disease is insidious, progressing over 10 to 20 years. Elevated liver enzymes and jaundice are indicative of late- stage hepatitis C infection. Often, asymptomatic carriers are undiagnosed until being identi- fied as positive during a blood-donor screening. Therapy for HCV includes a combination of interferon and ribavirin. Antiviral therapy is recommended for those at greatest risk of devel- oping cirrhosis. Policy Assess the employee in the occupational health unit and refer for medical evaluation if indi- cated. Hepatitis C Guideline continues on next page
Purchased from OEM Press by (ge corporate access). (C) 2013 OEM Health Information, Inc. All rights reserved.