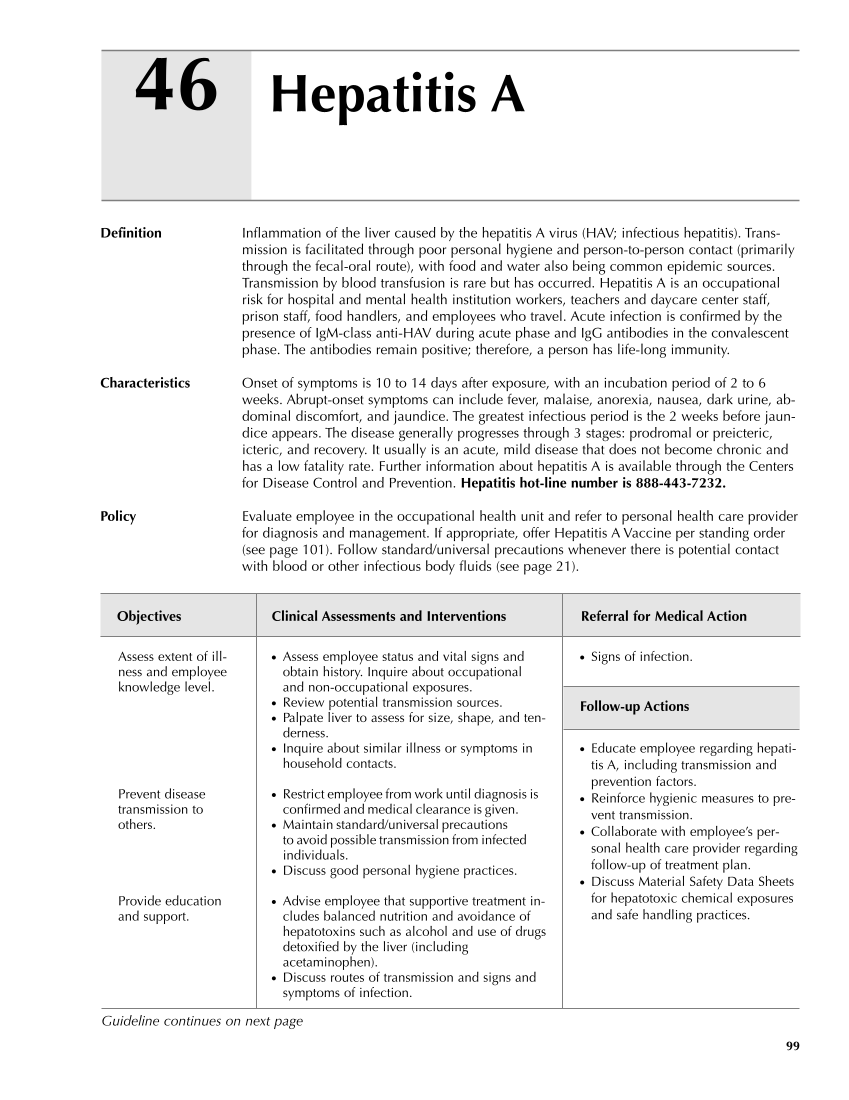
99 Hepatitis A 46 Definition Inflammation of the liver caused by the hepatitis A virus (HAV infectious hepatitis). Trans- mission is facilitated through poor personal hygiene and person-to-person contact (primarily through the fecal-oral route), with food and water also being common epidemic sources. Transmission by blood transfusion is rare but has occurred. Hepatitis A is an occupational risk for hospital and mental health institution workers, teachers and daycare center staff, prison staff, food handlers, and employees who travel. Acute infection is confirmed by the presence of IgM-class anti-HAV during acute phase and IgG antibodies in the convalescent phase. The antibodies remain positive therefore, a person has life-long immunity. Characteristics Onset of symptoms is 10 to 14 days after exposure, with an incubation period of 2 to 6 weeks. Abrupt-onset symptoms can include fever, malaise, anorexia, nausea, dark urine, ab- dominal discomfort, and jaundice. The greatest infectious period is the 2 weeks before jaun- dice appears. The disease generally progresses through 3 stages: prodromal or preicteric, icteric, and recovery. It usually is an acute, mild disease that does not become chronic and has a low fatality rate. Further information about hepatitis A is available through the Centers for Disease Control and Prevention. Hepatitis hot-line number is 888-443-7232. Policy Evaluate employee in the occupational health unit and refer to personal health care provider for diagnosis and management. If appropriate, offer Hepatitis A Vaccine per standing order (see page 101). Follow standard/universal precautions whenever there is potential contact with blood or other infectious body fluids (see page 21). Objectives Clinical Assessments and Interventions Referral for Medical Action ● Signs of infection. Follow-up Actions ● Educate employee regarding hepati- tis A, including transmission and prevention factors. ● Reinforce hygienic measures to pre- vent transmission. ● Collaborate with employee’s per- sonal health care provider regarding follow-up of treatment plan. ● Discuss Material Safety Data Sheets for hepatotoxic chemical exposures and safe handling practices. Assess extent of ill- ness and employee knowledge level. Prevent disease transmission to others. Provide education and support. ● Assess employee status and vital signs and obtain history. Inquire about occupational and non-occupational exposures. ● Review potential transmission sources. ● Palpate liver to assess for size, shape, and ten- derness. ● Inquire about similar illness or symptoms in household contacts. ● Restrict employee from work until diagnosis is confirmed and medical clearance is given. ● Maintain standard/universal precautions to avoid possible transmission from infected individuals. ● Discuss good personal hygiene practices. ● Advise employee that supportive treatment in- cludes balanced nutrition and avoidance of hepatotoxins such as alcohol and use of drugs detoxified by the liver (including acetaminophen). ● Discuss routes of transmission and signs and symptoms of infection. Guideline continues on next page
Purchased from OEM Press by (ge corporate access). (C) 2013 OEM Health Information, Inc. All rights reserved.