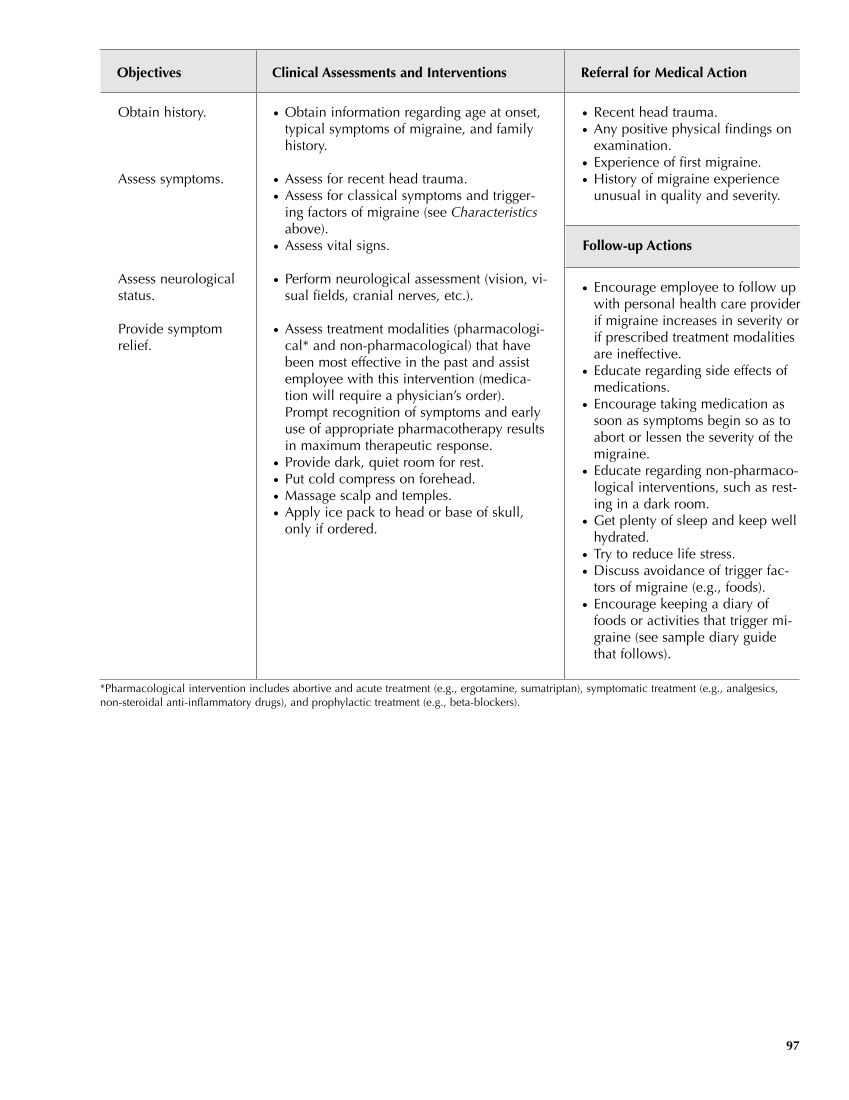
● Recent head trauma. ● Any positive physical findings on examination. ● Experience of first migraine. ● History of migraine experience unusual in quality and severity. Follow-up Actions ● Encourage employee to follow up with personal health care provider if migraine increases in severity or if prescribed treatment modalities are ineffective. ● Educate regarding side effects of medications. ● Encourage taking medication as soon as symptoms begin so as to abort or lessen the severity of the migraine. ● Educate regarding non-pharmaco- logical interventions, such as rest- ing in a dark room. ● Get plenty of sleep and keep well hydrated. ● Try to reduce life stress. ● Discuss avoidance of trigger fac- tors of migraine (e.g., foods). ● Encourage keeping a diary of foods or activities that trigger mi- graine (see sample diary guide that follows). Objectives Clinical Assessments and Interventions Referral for Medical Action 97 Obtain history. Assess symptoms. Assess neurological status. Provide symptom relief. ● Obtain information regarding age at onset, typical symptoms of migraine, and family history. ● Assess for recent head trauma. ● Assess for classical symptoms and trigger- ing factors of migraine (see Characteristics above). ● Assess vital signs. ● Perform neurological assessment (vision, vi- sual fields, cranial nerves, etc.). ● Assess treatment modalities (pharmacologi- cal* and non-pharmacological) that have been most effective in the past and assist employee with this intervention (medica- tion will require a physician’s order). Prompt recognition of symptoms and early use of appropriate pharmacotherapy results in maximum therapeutic response. ● Provide dark, quiet room for rest. ● Put cold compress on forehead. ● Massage scalp and temples. ● Apply ice pack to head or base of skull, only if ordered. *Pharmacological intervention includes abortive and acute treatment (e.g., ergotamine, sumatriptan), symptomatic treatment (e.g., analgesics, non-steroidal anti-inflammatory drugs), and prophylactic treatment (e.g., beta-blockers).
Purchased from OEM Press by (ge corporate access). (C) 2013 OEM Health Information, Inc. All rights reserved.